The Humana Healthcare Technology shift from prioritizing insurance to prioritizing healthcare allowed them to better understand the actual needs of customers, both present and future.
Have you understood the point we are trying to make? Sure. Let’s gain clarity by addressing this one question: How will you handle running an insurance company without your search platform while facing tough competition in your Medicare/Medicaid division, and navigating the healthcare industry transformed by a sudden global pandemic?
Throughout the COVID-19 outbreak, Humana, which ranks as the fourth largest insurance company in the US and is listed on the Fortune 500, faced this issue. Luckily, the backend work they completed prepared them to handle the challenges of digitalization, as stated at the Relevance 360 conference.
To fully understand the revamp of Humana Healthcare Technology, it is essential to look back at the pandemic era and understand the evolution of Humana Patient Technology.
Humana Healthcare Technology Rolls Out To Digitalization For Faster Response
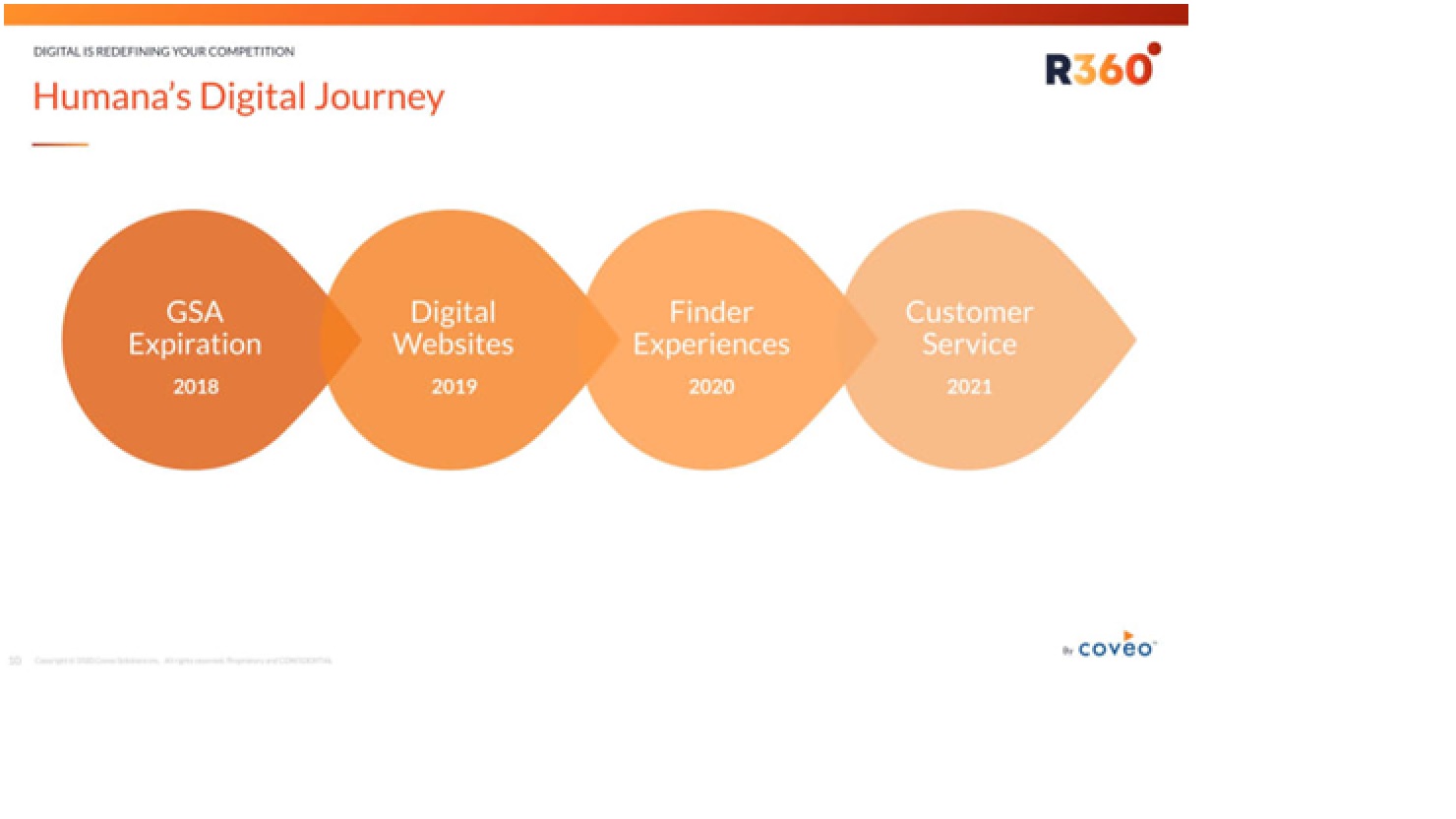
Humana Digital Health caters to customers from both the Medicare and Medicaid sectors, not just focusing on employer-based insurance providers. Since their business was closely linked to customers, it was essential to offer exceptional customer service and a high-quality digital experience to thrive. Because of this factor, Humana sought to swap out its Google Search Appliance for Humana Digital Health in 2018.
They tried products from various suppliers before deciding on a suitable platform. The primary goal of the project was to enhance the search functionality on their online platforms. Humana was aware that finding a doctor is one of the top three reasons customers visit their website. Because of this, the biggest insurance company decided to once more utilize and concentrate on the backend to introduce its Humana AI Healthcare dashboard for improving the user experience. These resources help patients find doctors, dentists, pharmacies, optometrists, and other healthcare professionals.
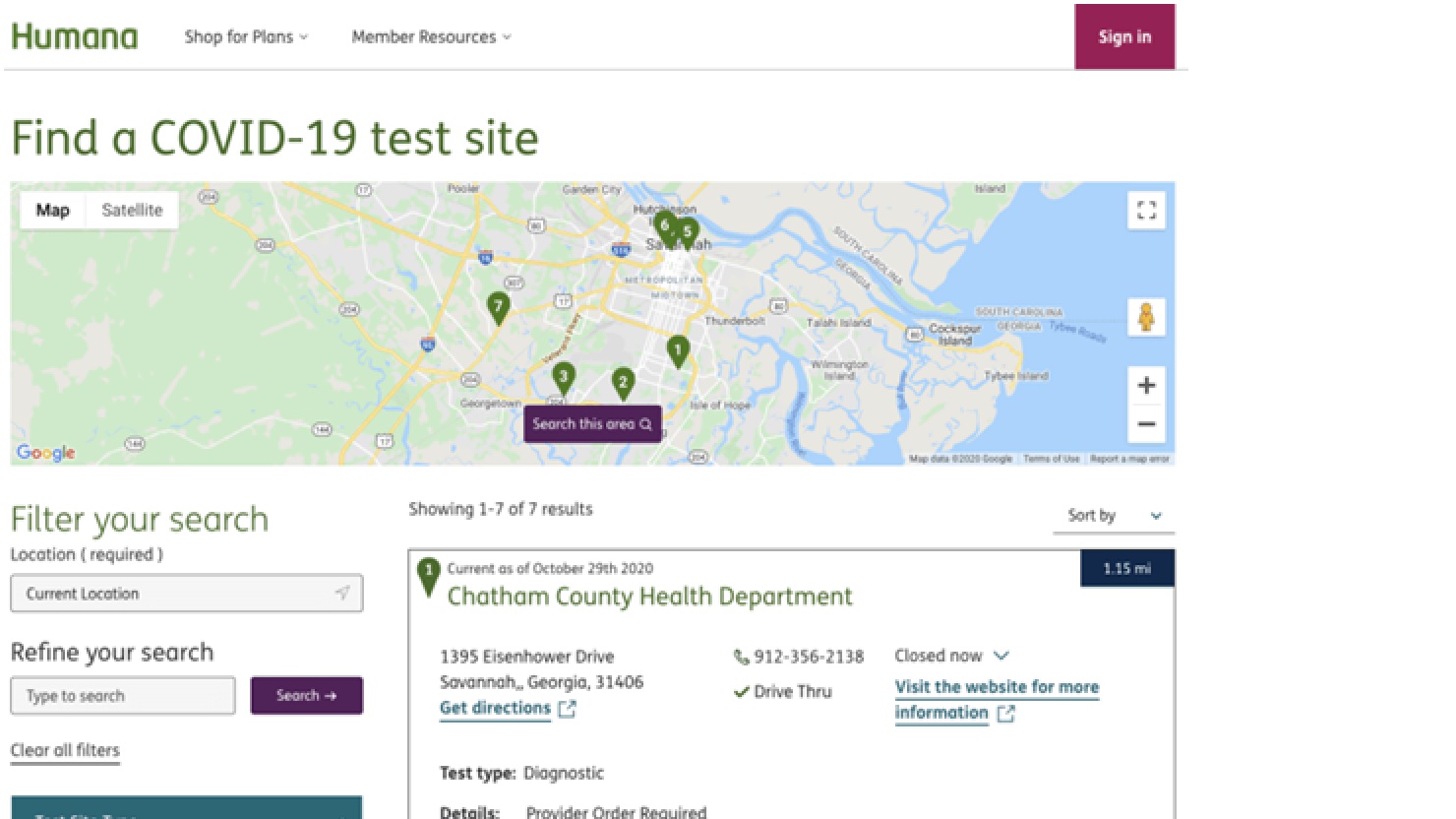
Nevertheless, this role became even more essential with the beginning of the pandemic and the rise of COVID-19. Humana once again considered quickly implementing a new search experience called Humana Telehealth for COVID-19 testing centers to address the urgent demand.
Implementation of Humana Telehealth During The Outbreak of COVID-19
The adoption of Humana telehealth was something of an overnight transition for the company. This was like a roadmap which the company thought of over like a three to five-year program as stated by the CEO.
Before COVID-19, there were about 14,000 telehealth sessions for Medicare recipients per week. Virtually overnight implementation of Humana Telehealth in a digital way accelerated this to 600,000 per week. That number is even higher when you include non-medicare customers.
Meanwhile, the US government authorized over 135 new telemedicine services and issued a waiver removing geographic restrictions. The pace of change in both regulations and how customers engage with accelerated Humana Patient Technology to a great extent. To adapt and make the most of these changes, Humana continuously worked to double down its efforts to provide an excellent digital experience and service to its customers and employees alike.
Key Benefits of Humana Healthcare Technology for Customers
The most prominent key benefits provided by Humana Digital Health during the outbreak of COVID-19 are:
- Humana eliminated member cost sharing for telemedicine and encouraged safe seeking of care.
- During the COVID-19 outbreak, they also expanded telehealth coverage and payment regulations.
- The payment for telehealth consultations matched that of in-person appointments.
- Audio-only phone calls were made available for individuals who do not have access to video calls.
- Different types of healthcare providers, such as primary care doctors and specialists were stressed to provide telehealth services by CMS and state regulations.
Apart from these initiatives Humana Telehealth also focused on key aspects like:
- Expenses for COVID-19 testing, including copays, coinsurance, deductibles, and healthcare facility visit costs, were no longer necessary as they were covered.
- Members could request early refills to ensure they had enough medication for prolonged periods, receiving an additional supply of 30 or 90 days as required.
- A dedicated hotline for members was set up, staffed with experienced call center agents who can assist with any queries and issues regarding the coronavirus, as well as offering personalized assistance for telehealth services.
Humana AI Healthcare Journey Begins Now
Humana incorporated AI into their site search during the COVID-19 outbreak to meet the needs of three web properties. Like Humana.com, HumanaMilitary.com, and MyHumana.com. The Humana AI Healthcare project involved incorporating information from the site’s current question-and-answer areas. Creating this question-answering feature proved to be more complex than a search bar due to the inclusion of context and various pathways.
After the first launch on Humana.com, analytics uncovered some fascinating discoveries. As the machine learning models were being trained during the rollout, the team included synonyms for typical mistakes such as “HIPA.” Manual adjustments made later on also involved the different labels for COVID-19.
“Making small adjustments like that helped us increase the click-through rate from 50% to around 60%,” Immerman said. Following these manual adjustments, the team activated machine learning, improved relevance, and provided query suggestions. In just three days, the percentage of people clicking through increased to 95%.
To work on the analytics and get proper and reliable results, Humana AI Healthcare executives and digital leaders utilized analytics to understand customer needs during the pandemic, creating a dashboard for specific search terms. They distributed 50 million free face masks based on customer intent and search volume by state.
What’s Next on The Humana Healthcare Technology Journey?
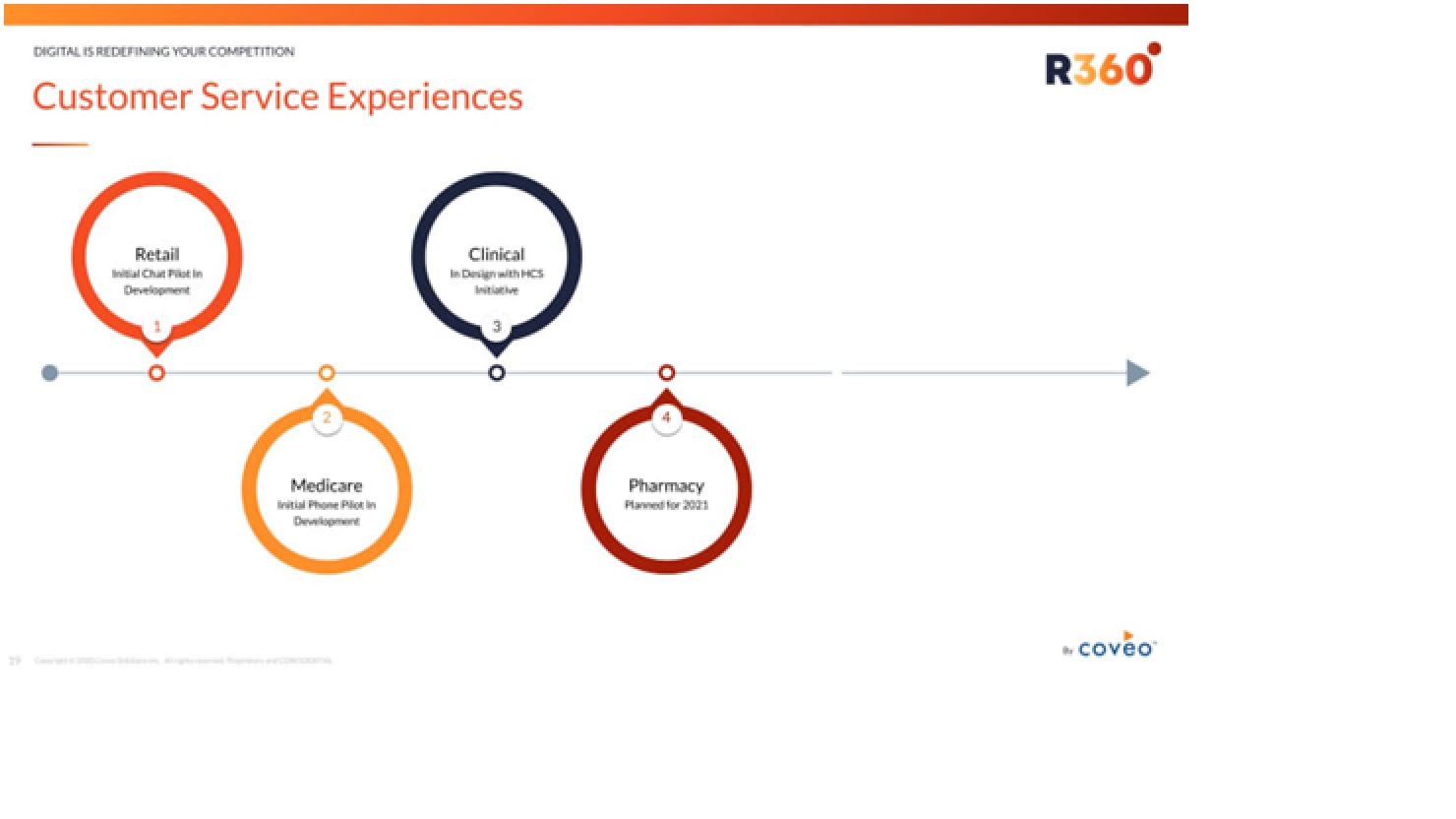
At present, Humana is concentrating on shifting its focus from being an insurance firm to becoming a “healthcare first” company. A new extensive effort is underway to establish clinical call centers within Humana Telehealth and Humana Patient Technology systems, offering support to doctors, nurses, and clinical staff through advanced search and machine learning tools.
At the same time, Humana is considering launching a new online digital pharmacy platform called Humana Pharmacy. The aim is to provide an organic search experience for clients, customer service representatives, and medical professionals similar to a Humana Digital Health system. This could be seen as a type of experience resembling “Google Ads” that provides customers with recommendations depending on their search situation.
The Bottom Line
In essence, Humana Healthcare Technology is anticipating prioritizing customer experience by utilizing the Coveo Relevance Platform. Humana remains focused on integrating all their data and utilizing analytics to understand customers’ current and future needs as they undergo transition.
For all the details about the latest health trends, medical news, and medical advancements, keep visiting DistilINFO HealthPlan: A Digital Way To Redefining The Health Updates.
FAQs
- What changes did Humana make to its technology in response to COVID-19?
Ans. Humana quickly put into place telehealth services, removed member expenses, increased coverage, and used AI to improve user satisfaction.
- What does the future hold for Humana Healthcare Technology?
Ans. Humana intends to create clinical call centers, introduce an online pharmacy platform, and focus on enhancing customer experience by integrating data and analytics.