Utilizing machine learning (ML) alongside mass spectrometry, UF Health researchers enhanced meningioma tumor assessment accuracy to 87%. Published in the Journal of the American Society for Mass Spectrometry, this study showcased ML’s prowess in refining tumor grading. By analyzing 85 samples, ML identified potential biomarkers, aiding in precise tumor characterization. Unexpectedly integrated into the study, ML expedited data analysis, evaluating 17,000 data points in seconds. This approach promises improved treatment guidance, especially for ambiguous grade II tumors, signaling a new frontier in personalized brain tumor care.
In a groundbreaking study published in the Journal of the American Society for Mass Spectrometry, researchers from the University of Florida (UF) Health have showcased a remarkable synergy between machine learning (ML) and liquid chromatography-high resolution mass spectrometry (LC-HRMS) to revolutionize the evaluation of brain tumors, particularly meningiomas. This innovative approach holds the promise of significantly improving tumor characterization accuracy, thereby aiding in more informed treatment decisions.
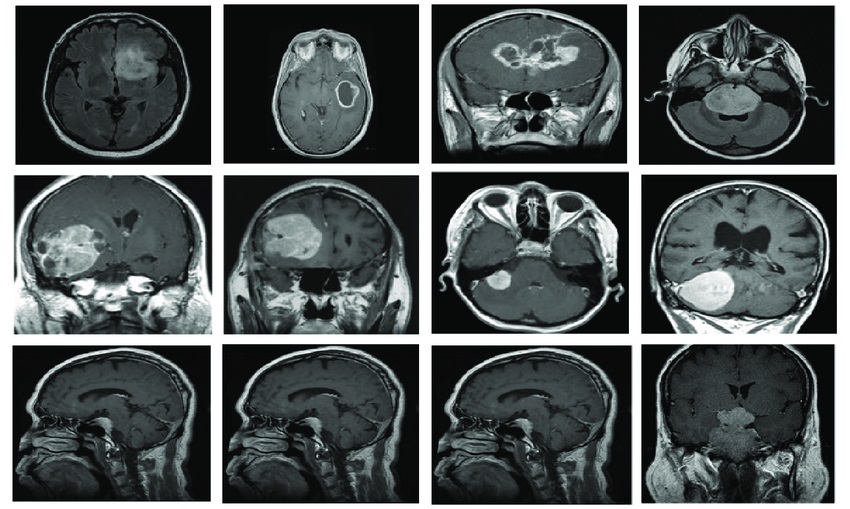
Meningioma tumors, classified as grade I, grade II, and grade III, often present a diagnostic challenge due to the complexities in distinguishing their severity. While grade I tumors typically progress slowly and are less menacing, grade III tumors are more aggressive, necessitating a combination of surgical removal and radiation therapy. The dilemma arises with grade II tumors, demanding a fine balance between observation and intervention.
Dr. Jesse L. Kresak, a co-author of the study and a clinical associate professor at UF’s College of Medicine, emphasized the ambiguity surrounding grade II tumors: whether to monitor them for potential recurrence or subject them to irradiation to prevent further growth.
To address this critical gap, the research team embarked on a comprehensive analysis of 85 meningioma samples using LC-HRMS, aiming to delve deeper into their metabolomic and lipidomic profiles. Surprisingly, the incorporation of ML was an unforeseen but transformative addition to their methodology.
Originally focused on identifying distinct chemical signatures to differentiate benign from malignant tumors, the researchers recognized the untapped potential of ML to unearth previously unseen patterns within the data. Dr. Timothy J. Garrett, another co-author and associate professor at the College of Medicine, highlighted how ML significantly enhanced the efficiency of tumor evaluation. ML-enabled the analysis of a staggering 17,000 data points in less than a second, a monumental leap from the conventional examination that assessed a mere 20 data points in ten minutes.
Despite the rapid processing of vast amounts of data, the accuracy remained strikingly high. One ML model displayed an initial accuracy rate of 87% in classifying tumor grades, hinting at the possibility of further refinement with larger sample sizes.
The implications of this research extend far beyond mere classification. The identified biomarkers and refined tumor characterization could potentially prompt the reclassification of tumors based on genetic makeup, leading to more personalized and effective treatment strategies for patients.
Dr. Kresak emphasized the importance of these tools in tailoring treatments for patients, underscoring their role in aligning the right treatment with the specific nature of the tumor.
This study stands as a testament to the transformative potential of data analytics and artificial intelligence (AI) in the field of oncology. Notably, the University of Texas MD Anderson Cancer Center recently established its Institute for Data Science in Oncology (IDSO) to leverage clinical expertise and data science in revolutionizing cancer care.
The IDSO aims to foster collaboration among various stakeholders, leveraging data-driven approaches to address the pressing needs of cancer patients. By enhancing data generation, collection, and management, MD Anderson aspires to usher in a new era of personalized care and improved patient experiences.
Overall, the amalgamation of ML and LC-HRMS techniques represents a monumental stride in brain tumor evaluation, particularly in the intricate realm of meningiomas. This research not only refines tumor characterization but also holds the potential to reshape treatment paradigms, marking a significant leap forward in the quest for more precise and personalized cancer care.




